13 Tips for Improving Patient Engagement
- Brett Fischer

- May 22, 2018
- 6 min read

I recently gave a talk during the Sanford Sports Medicine Symposium on patient engagement and multidirectional instability in the shoulder. I wanted to get some more thoughts down on the patient engagement side of things and be able to share for anyone interested. I feel like this is such an important part of what we do in healthcare – not just in physical therapy – yet, there isn’t a whole lot out there to learn from. Our typical healthcare research articles can leave a lot to be desired, but the business/marketing/branding arena is a great place to look for things that can carry over into physical therapy.
Much of the information I presented during my talk was from a book written by Daniel Pink, titled “To Sell is Human.” (I think I was tipped off on an Ask Mike Reinold podcast episode or from his blog somewhere along the line) Here is a more expanded version of what I talked about during that presentation.
The author starts out by reviewing the current stats for the workforce in the US, citing some research stating 1/9 jobs in the US are actually sales jobs (the type of job you think of when you hear the term “sales”), and the other 8/9 are what are referred to as “non-sales selling” jobs. Most healthcare jobs involving direct patient care fall into the non-sales selling category. Think of it this way: as a physical therapist, we are trying to motivate people to part with time and money in order for them to work on some things that will help them feel better.
We all know that we are trying to help our patients reach their goals – but – what about all the other times we function in a non-sales selling role? We have to convince administrators of our worth as a profession. We have to help coaches and players realize there may be a better way to warm up or manage the game in an effort to reduce injury. We have to talk with parents and help them decide what’s best for their kids. We participate in efforts to educate the public (and other professionals) on what we are capable of as a profession. It’s a constant battle.
When we think about all those people needing convincing, it can be a bit overwhelming. But the author then presents us with a few manageable tactics – the new ABCs: attunement, buoyancy, and clarity. Attunement can be thought of as a feeling of connectivity with another person. Buoyancy is a resiliency of spirit and cheerfulness, or positivity. Clarity meaning you’ve kept a good perspective.
Next, a few tips on each of the ABCs are given and these truly apply to anyone working with patients. Especially those of us who are trying to encourage behavior change or modification.
Attunement – Connect!
Begin as a person of lower power. Be at their level sit down in front of them, but not directly in front, sit off to an angle, this makes it less direct and confrontational.
Keep perspective. Remember each patient has a life outside of therapy. Don’t forget to ask, “how is your day going?”.
Selective Mirroring. Inconsistent mimicking can be effective in connecting with people. As humans, we are already programmed to do this, so don’t try too hard on this. Pay attention the next time you are people watching and you’ll see what he is referring to.
Small talk. “Search for similarities: We dismiss this as small talk but that’s a mistake. Similarity – the genuine, not the manufactured variety – is a key form of human connection, people are more likely to move together when they share common ground.” BE GOOD AT GENUINE SMALL TALK. This is important.
(Not mentioned in the book): Know three things about each patient that have nothing to do with why you’re seeing them. This is a great way to prove that you’ve connected on a level that will be helpful for you and the patient.
Buoyancy – Positivity!
Declarative v. Interrogative self talk. Am I the only one that wakes up in the morning and says to myself in the mirror “I look good today!” Turns out according to the author I should be saying “Do I look good today?”. Phrasing this as a question is a way of making yourself or others come up with confirmation, instead of just blindly believing the statement.
Monitor your positivity ratio. A great ratio for positive to negative comments is 3:1. (For more information, head to Dr. Barbara Fredrickson’s web site here for a free calculator, it only takes a couple minutes.) More positivity than that and it looks blindly optimistic, which can turn your patient the other way. Keep in mind how challenging it is to be in PT. For instance, if you have a patient that’s three weeks out from his ACL reconstruction, extension is looking great, but his quad is not responding the way you think it should by now. What do we do? We focus on that quad a little more and on the extension a little less. That process can be tough for some patients to handle. We are always working on improving areas that may be lagging behind, but that can feel quite negative if you aren’t explaining it as a process to the person in front of you. I’ve tried to be more conscious of this in the past couple years and I think it’s been helpful in maintaining a good relationship with my patients and keeping them going down the right road.
Be conscious of emotions in the moment. The author recommends keeping some positive emotions (joy, gratitude, serenity, interest, hope, pride, amusement, inspiration, awe, and love) in the front of your mind as a way to make sure you recognize them as they happen throughout your day. Maybe you keep them on a sticky note in your office somewhere or as a reminder on your phone.
Turn negative events into positives. This one can be a struggle for me. Try asking yourself these questions the next time something negative happens:
Is this permanent?
Is this pervasive?
Is this personal?
The chances are, the answers to these questions will be no. Forcing yourself to answer those questions can help your mind be at ease. (See first bullet point above.)
Dispute and de-catastrophize negative events. To me this sounds like coming up with excuses, but honestly there’s a difference between excuses and reasons. Here, we’re just coming up with reasons why we can do better the next time.
“I haven’t been getting enough sleep lately.”
“I should have known more about that injury.”
Clarity – Understanding!
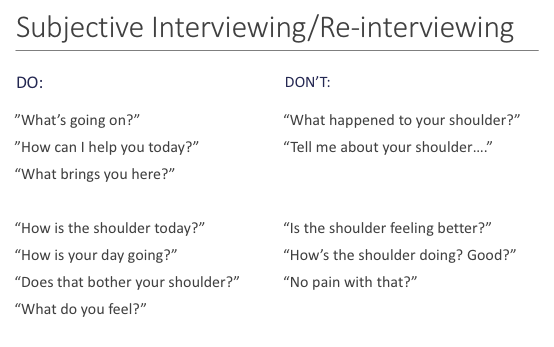
Learn how to ask better questions. (See below). This is something I've really paid more attention to in the last year or so. I constantly am trying to be better at how I phrase my questions to get the most clear picture of what the patient is experiencing. It's critical, because that feedback drives your decision making for that patient for that day and beyond.
Sometimes you need a jolt. Clarity is all about gaining perspective and helping your patient gain some perspective. This involves getting out of your normal routine every now and again. A mini jolt might include taking a new route to work, sitting in a different spot at work or in a class, or trying a new food. A half jolt would be observing a different job role for a day, driving a different car, or getting a more extreme haircut. The full jolt is simply jumping into a whole new culture. Any of these can be effective at the right time.
Help other people find some perspective. We’ve all had patients who just aren’t into being in PT, whether it’s a 15 year old being drug to the clinic by her parents or otherwise. Rational questions are sometimes ineffective for motivating resistant people, instead, irrational questions may motivate them better. For example, I asked my oldest daughter the other day while she was whining on our way to the ballpark for softball practice: “on a scale of 1-10, how ready are you to practice some softball tonight?” She responded by saying 1. I then said “why not lower?”. She then said “OK fine, 0.” Apparently this doesn’t work well for my 9 year old, but I think this can help open your patients’ eyes to why they might be able to give up some time and effort to work on a few exercises throughout the day.
The author goes on to discuss pitch, improvisation, and service as the last three keys to moving people. These are also important points for us in healthcare, however, I really feel like the ABCs are the bread and butter for us. I’d highly recommend checking out this book or even trying a few of the things mentioned above.
What strategies have you used with your patients? What’s worked for you?
Brett

Comments